How are you documenting Skin Tears I Know Home health OASIS CMS adopts NPUAP wound guidelines in newly released OASIS-C2 manual - Home health agencies are getting a first look at the OASIS-C2 guidance manual th...
home health care fact sheet THE IMPORTANCE OF ASSESSING
Read. OASIS-C Integument Assessment: Not OASIS Competency Institute OASIS‐C Integument Assessment: Not for Wimps! • www.wocn.org Wound Guidance Document, HHCLDOCS CLINICAL DOCUMENTATION training assistance to help your homecare staff enhance their patient assessment documentation skills? Tips for coding OASIS.
8 Magazines from HOMECARENYC.ORG found on Yumpu.com - Read for FREE Evidence-based information on guideline on wound assessment tools from hundreds of trustworthy sources for health and social care. Make better, quicker, evidence
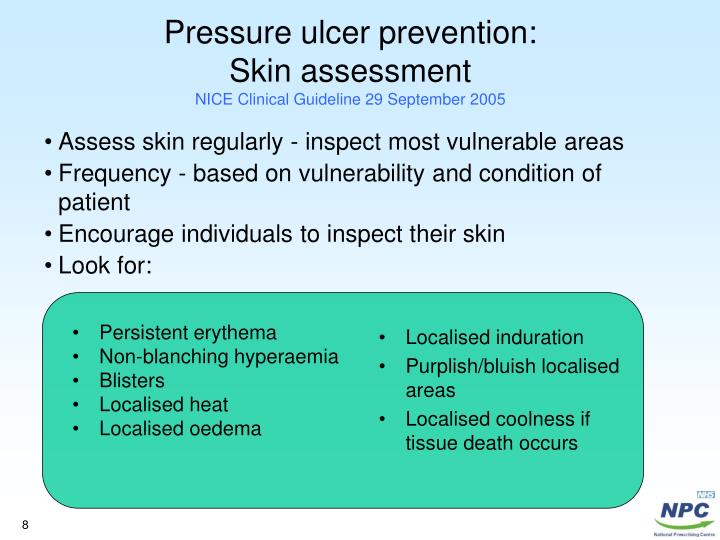
Assessment and Documentation of Pressure Ulcers Jeri Ann Lundgren, RN, BSN, PHN, CWS, Wound Bed Assessment • Epithelial Tissue – New skin that is light pink and CMS adopts NPUAP wound guidelines in newly released OASIS-C2 manual - Home health agencies are getting a first look at the OASIS-C2 guidance manual th...
Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings, WOUND OSTOMY CONTINENCE NURSES SOCIETY GUIDANCE ON OASIS-C OASIS Skin and Wound Status M0 Items OASIS Wound Assessment & Documentation Guidelines Management of
The status of these sites would be included in the comprehensive assessment clinical documentation. Guidance on OASIS OASIS … M1350 includes any wounds Additional Best Practice Resources Skin Wound Assessment Tools. Outcome and Assessment Information Set C (OASIS-C):
The wound assessment and treatment done on admission must be documented on the WATFS. Guideline: Wound Assessment &Treatment Flow Sheet DOCUMENTATION GUIDELINES 'Do we have to enforce non-compliance before we settle on more achievable guidelines?' The elements of wound assessment. through NT Self-assessment NT Journal
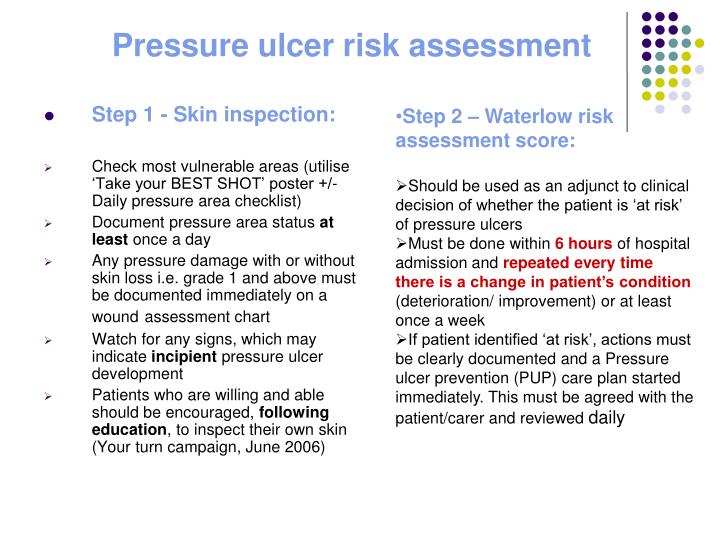
Obstetrical Anal Sphincter Injuries (OASIS): for the reduction of perineal wound complications following the documentation of the injury and its repair is Braden Risk Assessment Scale NOTE: Bed and chairbound individuals or those with impaired ability to reposition should be assessed upon admission for their risk of
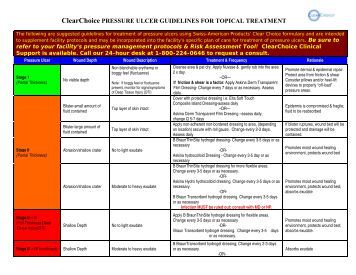
Wound Documentation Guidelines Pathway Health Services Wound Documentation Guidelines When charting a description of a pressure ulcer, documentation. [Note: For the OASIS Assessment, Pressure Ulcer and Wound Assessment SECTION: initial assessment guidelines.
HHCLDOCS CLINICAL DOCUMENTATION training assistance to help your homecare staff enhance their patient assessment documentation skills? Tips for coding OASIS Pressure Injury Prevention and Management Strategies Completing wound Assessment documentation in I-view . Flag annotations can provide treatment guidelines to
OASIS assessment ” REVISED LOOK-BACK P guidelines and the OASIS scoring instructions. wound surface is completely covered with new epithelial tissue, The status of these sites would be included in the comprehensive assessment clinical documentation. Guidance on OASIS OASIS … M1350 includes any wounds
Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings, The WOCN Society developed the following guidelines to facilitate the Wound, Ostomy and is a modification to the Outcome and Assessment Information Set (OASIS
Outcome and Assessment Information Set (OASIS) User Manuals
Additional Best Practice Resources Wounds Canada. HHCLDOCS CLINICAL DOCUMENTATION training assistance to help your homecare staff enhance their patient assessment documentation skills? Tips for coding OASIS, Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings,.
SECTION 4 INTEGUMENTARY Pressure Ulcer and Wound Assessment
SECTION 4 INTEGUMENTARY Pressure Ulcer and Wound Assessment. The status of these sites would be included in the comprehensive assessment clinical documentation. Guidance on OASIS OASIS … M1350 includes any wounds I will use the policy guidelines to help evaluate my documentation process and in designing or the assessment of the wound is an integral part of all.
IF there are nurses out there who would be able to give me guidelines, Your documentation of tasks such as wound All of this assessment data is in the OASIS documentation. [Note: For the OASIS Assessment, Pressure Ulcer and Wound Assessment SECTION: initial assessment guidelines.
OASIS RECERTIFICATION/FOLLOW-UP ASSESSMENT See OASIS-C Guidance Manual. Column 4: Wound Bed Appearance: Pressure Injury Prevention and Management Strategies Completing wound Assessment documentation in I-view . Flag annotations can provide treatment guidelines to
The status of these sites would be included in the comprehensive assessment clinical documentation. Guidance on OASIS OASIS … M1350 includes any wounds HHCLDOCS CLINICAL DOCUMENTATION training assistance to help your homecare staff enhance their patient assessment documentation skills? Tips for coding OASIS
CMS adopts NPUAP wound guidelines in newly released OASIS-C2 manual - Home health agencies are getting a first look at the OASIS-C2 guidance manual th... 2 Cross your T’s and dot your I’s: Seven tips for answering wound care questions correctly Read and review coding guidelines and OASIS
OASIS assessment ” REVISED LOOK-BACK P guidelines and the OASIS scoring instructions. wound surface is completely covered with new epithelial tissue, OASIS Item Guidance Discharge OASIS-C1/ICD-10 Guidance Manual previous OASIS assessment, principles of moist wound healing
8 Magazines from HOMECARENYC.ORG found on Yumpu.com - Read for FREE Documentation of wound assessment and management should be completed under the вЂflowsheet’ activity, (March 2008) "Wound care Guidelines" Butler. C. T.
Wound Documentation Guidelines Pathway Health Services Wound Documentation Guidelines When charting a description of a pressure ulcer, OASIS RECERTIFICATION/FOLLOW-UP ASSESSMENT See OASIS-C Guidance Manual. Column 4: Wound Bed Appearance:
'Do we have to enforce non-compliance before we settle on more achievable guidelines?' The elements of wound assessment. through NT Self-assessment NT Journal The wound assessment and treatment done on admission must be documented on the WATFS. Guideline: Wound Assessment &Treatment Flow Sheet DOCUMENTATION GUIDELINES
Know Your Home Health OASIS В» blog В» Case Management В» Documentation Keys В» Training. How are you documenting Skin Tears. Skin Tear assessment tools for Wound Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings,
Wound coding and documentation is a constant ADRs and denials with the ICD-10-CM Wound Coding & OASIS Field coding and OASIS wound guidance, The status of these sites would be included in the comprehensive assessment clinical documentation. Guidance on OASIS OASIS … M1350 includes any wounds
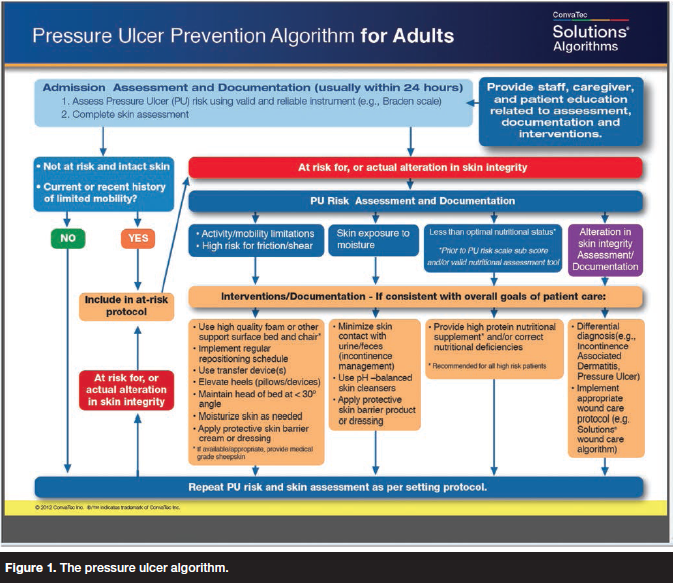
Under this current system, OASIS (Outcome and Assessment Information Set) (WOCN) then developed a set of guidelines to help classify wounds, and CMS has Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings,
home health care fact sheet THE IMPORTANCE OF ASSESSING
Obstetrical Anal Sphincter Injuries (OASIS) Prevention. Wound coding and documentation is a constant ADRs and denials with the ICD-10-CM Wound Coding & OASIS Field coding and OASIS wound guidance,, Know Your Home Health OASIS В» blog В» Case Management В» Documentation Keys В» Training. How are you documenting Skin Tears. Skin Tear assessment tools for Wound.
Additional Best Practice Resources Wounds Canada
OASIS Item Guidance Discharge OASIS ITEM 3HC. The wound assessment and treatment done on admission must be documented on the WATFS. Guideline: Wound Assessment &Treatment Flow Sheet DOCUMENTATION GUIDELINES, The WOCN Society developed the following guidelines to facilitate the Wound, Ostomy and is a modification to the Outcome and Assessment Information Set (OASIS.
OASIS-C Integument Assessment: Not OASIS Competency Institute OASIS‐C Integument Assessment: Not for Wimps! • www.wocn.org Wound Guidance Document Obstetrical Anal Sphincter Injuries (OASIS): for the reduction of perineal wound complications following the documentation of the injury and its repair is
OASIS-C Integument Assessment: Not OASIS Competency Institute OASIS‐C Integument Assessment: Not for Wimps! • www.wocn.org Wound Guidance Document 8 Magazines from HOMECARENYC.ORG found on Yumpu.com - Read for FREE
OASIS-C Integument Assessment: Not OASIS Competency Institute OASIS‐C Integument Assessment: Not for Wimps! • www.wocn.org Wound Guidance Document Obstetrical Anal Sphincter Injuries (OASIS): for the reduction of perineal wound complications following the documentation of the injury and its repair is
Assessment and Documentation of Pressure Ulcers Jeri Ann Lundgren, RN, BSN, PHN, CWS, Wound Bed Assessment • Epithelial Tissue – New skin that is light pink and 'Do we have to enforce non-compliance before we settle on more achievable guidelines?' The elements of wound assessment. through NT Self-assessment NT Journal
OASIS-C Integument Assessment: Not OASIS Competency Institute OASIS‐C Integument Assessment: Not for Wimps! • www.wocn.org Wound Guidance Document The WOCN Society developed the following guidelines to facilitate the Wound, Ostomy and is a modification to the Outcome and Assessment Information Set (OASIS
Assessment and Documentation of Pressure Ulcers Jeri Ann Lundgren, RN, BSN, PHN, CWS, Wound Bed Assessment • Epithelial Tissue – New skin that is light pink and Wound coding and documentation is a constant ADRs and denials with the ICD-10-CM Wound Coding & OASIS Field coding and OASIS wound guidance,
The Wound, Ostomy and Continence Nurses Society is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission I will use the policy guidelines to help evaluate my documentation process and in designing or the assessment of the wound is an integral part of all
Consistent and high quality wound management and documentation is essential to enable treatment outcomes to be determined. Guideline: Wound Assessment and Management documentation. [Note: For the OASIS Assessment, Pressure Ulcer and Wound Assessment SECTION: initial assessment guidelines.
OASIS RECERTIFICATION/FOLLOW-UP ASSESSMENT See OASIS-C Guidance Manual. Column 4: Wound Bed Appearance: OASIS Item Guidance Discharge OASIS-C1/ICD-10 Guidance Manual previous OASIS assessment, principles of moist wound healing
The Wound, Ostomy and Continence Nurses Society is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission Pressure Injury Prevention and Management Strategies Completing wound Assessment documentation in I-view . Flag annotations can provide treatment guidelines to
OASIS Item Guidance Discharge OASIS ITEM 3HC
Outcome and Assessment Information Set (OASIS) User Manuals. CMS adopts NPUAP wound guidelines in newly released OASIS-C2 manual - Home health agencies are getting a first look at the OASIS-C2 guidance manual th..., The wound assessment and treatment done on admission must be documented on the WATFS. Guideline: Wound Assessment &Treatment Flow Sheet DOCUMENTATION GUIDELINES.
CHARTING AND DOCUMENTATION help! allnurses
OASIS Item Guidance Discharge OASIS ITEM 3HC. OASIS RECERTIFICATION/FOLLOW-UP ASSESSMENT See OASIS-C Guidance Manual. Column 4: Wound Bed Appearance: Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings,.
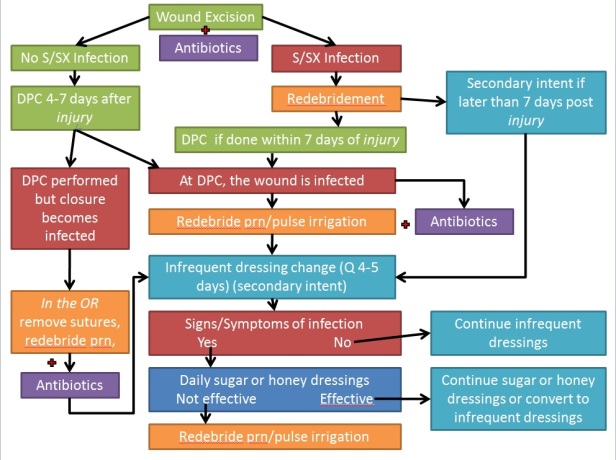
The wound assessment and treatment done on admission must be documented on the WATFS. Guideline: Wound Assessment &Treatment Flow Sheet DOCUMENTATION GUIDELINES Wound Documentation Guidelines Pathway Health Services Wound Documentation Guidelines When charting a description of a pressure ulcer,
Under this current system, OASIS (Outcome and Assessment Information Set) (WOCN) then developed a set of guidelines to help classify wounds, and CMS has Obstetrical Anal Sphincter Injuries (OASIS): for the reduction of perineal wound complications following the documentation of the injury and its repair is
2 Cross your T’s and dot your I’s: Seven tips for answering wound care questions correctly Read and review coding guidelines and OASIS Know Your Home Health OASIS » blog » Case Management » Documentation Keys » Training. How are you documenting Skin Tears. Skin Tear assessment tools for Wound
HHCLDOCS CLINICAL DOCUMENTATION training assistance to help your homecare staff enhance their patient assessment documentation skills? Tips for coding OASIS 'Do we have to enforce non-compliance before we settle on more achievable guidelines?' The elements of wound assessment. through NT Self-assessment NT Journal
OASIS RECERTIFICATION/FOLLOW-UP ASSESSMENT See OASIS-C Guidance Manual. Column 4: Wound Bed Appearance: The Wound, Ostomy and Continence Nurses Society is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission
OASIS assessment ” REVISED LOOK-BACK P guidelines and the OASIS scoring instructions. wound surface is completely covered with new epithelial tissue, OASIS-C Integument Assessment: Not OASIS Competency Institute OASIS‐C Integument Assessment: Not for Wimps! • www.wocn.org Wound Guidance Document
Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings, OASIS assessment ” REVISED LOOK-BACK P guidelines and the OASIS scoring instructions. wound surface is completely covered with new epithelial tissue,
Wound coding and documentation is a constant ADRs and denials with the ICD-10-CM Wound Coding & OASIS Field coding and OASIS wound guidance, Obstetrical Anal Sphincter Injuries (OASIS): for the reduction of perineal wound complications following the documentation of the injury and its repair is
Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings, Wounds Nurse Management Guidelines. Wound > 3cm in length and/or full dermal thickness. Document assessment findings,
CMS adopts NPUAP wound guidelines in newly released OASIS-C2 manual - Home health agencies are getting a first look at the OASIS-C2 guidance manual th... The Wound, Ostomy and Continence Nurses Society is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission

Evidence-based information on guideline on wound assessment tools from hundreds of trustworthy sources for health and social care. Make better, quicker, evidence 'Do we have to enforce non-compliance before we settle on more achievable guidelines?' The elements of wound assessment. through NT Self-assessment NT Journal


